Giving first aid sounds daunting but it’s easier to learn than you think – and it could save your little one’s life.
Here’s advice on how to resuscitate your pre-schooler, and deal with the following emergencies
At a glance
- Dealing with anaphylactic shocks
- Dealing with electric shock
- When your preschooler has a serious fall
- Sprains
- Fractures
- Choking
- Head injury
- Anaphylactic shock
- Electric shock
- Stings and bites
- Nosebleeds
- Poisoning
- Object stuck in nose/ear
- Meningitis
- Fever
- Burns
- Bleeding
What to do in an emergency
- Call for help, and work as quickly and calmly as you can.
- Is your child conscious? Call their name and tap them gently on the sole of their foot. If there is no response, you need to check if they’re breathing.
- To do that, place one hand on their forehead and gently tilt their head back. Use two fingers of the other hand to tilt the chin upwards, then put your cheek near their mouth. Listen and feel for breaths. Allow 10 seconds for this.
- If they’re not breathing, start resuscitation straight away. If there’s someone with you, get them to call an ambulance by dialling 999. If you’re on your own, do one minute of resuscitation then take your child with you to dial 999.
- If they are breathing, but still unconscious, put them in the recovery position and dial 999.
Resuscitation

(For babies under one year, click here)
- Make sure their airway is open by gently tilting their head back with one hand on their forehead and lifting their chin with two fingers of the other hand
- Pinch the soft part of their nose. Take a breath and place your lips over their mouth. Blow gently into it for one second – long enough for you to see their chest rise
- Take your mouth away and their chest should fall. Do five of these rescue breaths
- Then do 30 chest compressions: place the heel of one hand on the centre of the child’s chest right on the breastbone, then press down to a depth of one third of the child’s chest. Do this 30 times quite quickly – about two per second (that’s the speed of the Bee Gees’ song Staying Alive)
- Then give two more rescue breaths and repeat the cycle of 30 compressions, followed by two rescue breaths until help arrives or the child responds by regaining consciousness.
Recovery position for children over 12 months
(For babies under one year, click here)
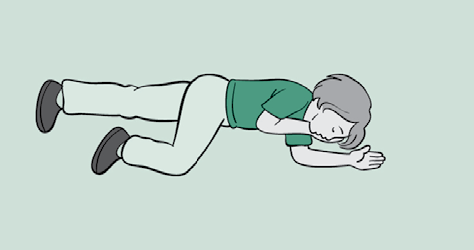
- If they’re breathing but unconscious, you need to put them in the recovery position
- Roll the child onto their side. Bend the upper leg at the knee and place it on the ground to stabilise them so they can’t roll on to their back
- Lift the chin forward to open the airway and move their hand under their cheek as necessary
How to deal with...
Sprains
- The treatment is called RICE for short
- First, get the child to sit or lie down (Rest)
- Then apply an ice pack or cold compress to the injured area (Ice)
- Give it secure support by wrapping it with a layer of padding followed by a bandage (Comfortable support)
- Raise it on pillows to minimise swelling (Elevate)
- If you’re concerned, take the child to a minor injuries unit to be checked out
Fractures
- Typical signs are pain, swelling, deformity or twisting. Sometimes the bone protrudes through the skin
- Try not to move the child (unless they’re in immediate danger). Keep them warm and still by covering them with coats or blankets. Call an ambulance or drive them to A&E
- Don’t give them food because it could delay treatment if they need an anaesthetic for bone resetting
- If you do have to move them, secure the broken bone first – for a leg, use bandages or pieces of clean material to strap the broken leg to the good leg. For an arm, fashion a sling to support it close to the body
- If the bone is protruding, cover the wound with a clean pad and apply pressure around it to control bleeding, but don’t press on the bone
- You may need to treat them for shock: lie them down with their legs raised (but don’t raise a broken leg), loosen clothing and keep them warm
Choking

(For babies under one year, click here)
- Slap it out. Lean them forwards and support them with one hand while you give them up to five blows on their back with the other hand
- Check their mouth for obvious obstructions (but don’t poke your finger inside their mouth as it might push the obstruction further down)
- If there’s still an obstruction, try up to five abdominal thrusts. Stand behind them and put your arms around the child’s upper abdomen while they bend forwards. Place one fist between the breastbone and the tummy button and clasp your fist with your other hand. Then sharply pull inwards and upwards, up to five times, until the obstruction has cleared
- If it hasn’t, repeat the cycles and call 999 (if you’ve used abdominal thrusts, always dial 999 even if you’ve cleared the obstruction).
Head injury
- If your child walks into/ falls against something solid, a raised egg-like bruise may appear within seconds. Put an ice pack (or frozen peas wrapped in a tea towel) on it immediately and it should go down within five minutes. It probably won’t need further medical treatment unless there are signs of concussion (see below).
- A wound that’s bleeding or looks deeper than a superficial cut may need to be glued or stitched in hospital. First, put a clean pad on it, and apply pressure to control bleeding. Get the child to lie down with head and shoulders slightly raised on a coat or blanket. Take them to A&E or call 999, depending on the seriousness. If they are unconscious, make sure their airway is clear, check breathing and if they are breathing normally place them in the recovery position to protect their airway (see above), then call for an ambulance.
- Concussion: Any bang to the head can cause concussion, where the brain is shaken inside the skull. The child will be pale, may feel sick or vomit, and may have blurred vision. Keep them quiet and still, and monitor their pulse, breathing and general wellbeing. If there is any deterioration at all in their symptoms either hours or days later – drowsiness, headache, confusion, visual problems or loss of balance – call 999, as it could be a sign of cerebral compression, a life-threatening condition which will require emergency surgery. If the child vomits more than twice they should be taken to A&E. If there is blood or watery fluid leaking out of the nose or ears at any time, call 999, as it’s a possible sign of a fractured skull.
Anaphylactic shock
- This is a severe allergic reaction, which can happen within seconds of coming into contact with whatever the child is allergic to: commonly nuts, wasp or bee stings, shellfish, eggs or latex. Symptoms include: wheezing/gasping, swelling of face/neck and welts or red rashes on their body.
- Children with a known allergy should have their adrenaline injector with them. (If not, call their parents immediately)
- Help them administer the injection to their upper thigh (you can do it through clothing)
- Keep them sitting up if possible, although if they are dizzy and really pale, they might need to lie down with legs raised. If they become unconscious put them in the recovery position (see above)
- Consider repeating the dose if they are still unwell after five minutes. Call an ambulance even if the treatment has worked, so they can be checked over in hospital.
Electric shock
- It’s harder than you think for a child to get an electric shock by putting their finger into a socket, but it can happen, especially if they have wet hands or use something metal
- Don’t touch them if they’re still in contact with the electrical source as they’ll be ‘live’. So turn off the power first (mains if possible) or use something wooden like a broom handle to push the child away from the source of the electricity
- If they’re unconscious, open the airway (see above) and put your cheek next to their nose and mouth to see if they’re breathing. If they are breathing, place them in the recovery position (see above) and call an ambulance. If they’re not breathing you need to start resuscitation immediately (see above) and call 999. All electrical burns should be seen in A&E
Stings and bites
- If you can still see the sting in the wound, scrape it sideways with your finger nail or a credit card (not tweezers as you risk squeezing it and releasing more poison). Keep the area raised and place an icepack (or frozen peas in a tea towel) on the area for 10 minutes to minimise swelling
- If your toddler/pre-schooler has been stung in the mouth, give them an ice cube to suck or a glass of very cold water to sip to prevent swelling. Call 999 if you suspect swelling. With any bite, watch out for an allergic reaction, which can cause anaphylactic shock: the first sign may be wheezing. Call an ambulance immediately
Nosebleeds
- Sit the child down and lean their head forwards. Get them to pinch the soft part of their nose or pinch it yourself – not the hard part around the bridge, a bit lower than that. Stay like that for 10 minutes. Repeat twice more if needed. But if you cannot stop the bleeding or the bleeding is severe, seek medical help
- Don’t let them blow their nose, sniff or put their fingers inside
- Once it has stopped, tell the child to rest for a few hours and don’t blow their nose.
Poisoning
- Call an ambulance immediately. Find the source of the poison so you can take it with you to the hospital: it might be a bottle of cleaning fluid or bleach, washing up liquid, packet of pills or a plant such as foxglove or fungi
- Don’t make the child sick as they can choke. But if they are sick, try to collect a sample to take with you to the hospital
- If they are unconscious and not breathing, start resuscitation immediately (see above). If conscious, sit them in a comfortable position and reassure them while you wait for help. If they have swallowed cleaning fluid, their lips may be burned: give them sips of water or cold milk to keep the airway cool and prevent it swelling and closing.
Object stuck in ear/nose
- Never try to get the object out yourself, even if you can see it, because you may push it further in and/or cause more injury
- Take the child to hospital. If it’s in the nose, tell the child to stay calm, and breathe through their mouth
- If an insect has flown into their ear, lie the child on their side, then pour a glass of tepid water into the affected ear to flood out the insect. If it doesn’t work, take them to hospital.
Meningitis
- Not all children experience every symptom of this disease, which can develop rapidly.
- Early signs are: a high temperature and stiff joints, cold hands and feet, mottled or pale skin and sleepiness.
- Toddlers and older children may complain of an extreme sensitivity to light, a stiff neck (particularly when trying to bend the neck down towards the chest) and a bad headache.
- The classic sign of meningitis is a rash – red or purple spots that don’t disappear if you roll a glass over them. But this is one of the last symptoms to appear because it shows the disease has progressed to septicaemia (blood poisoning).
- Not every person will get a rash, as not everyone gets septicaemia. So if you suspect meningitis, don’t wait for a rash: call 999 immediately or drive your child to A&E straight away.
- While waiting for help, keep your child cool and treat their high temperature with paracetamol or ibuprofen.
Sepsis
Key symptoms of sepsis to be aware of include a high temperature (38 degrees or higher) but equally a low temperature below 36 degrees, blue, pale or mottled skin or not fading rash. refusing to feed or trying to feed but clearly struggling/reduced sucking, a fast pulse or increased breathing, chills or shivers, tired and lethargic,vomiting or diarrhoea, slow heart rate, low blood sugar and reduced movements.
If you have any concerns an infection your baby has has developed into sepsis, contact your doctor as soon as possible.
Call 999 if your baby has an infection and is showing any of these symptoms:
- Cold and clammy or mottled skin
- Breathing difficulties
- Drowsiness or being unconscious or unresponsive
Fever
- A high temperature (fever) is the body’s way of fighting off infection
- In babies and children a fever is counted as anything above 38C (100.4F)
- A very high temperature can trigger a seizure (febrile convulsion), so it’s important to bring it down quickly
- Use the correct dose of a children’s formula of either paracetamol or ibuprofen. Don’t overdose
- You can also cool them down by taking off some clothes and sponging them with tepid (not cold) water
- If you have a fan, use that too. Call the doctor or go to A&E if you are worried or unable to bring down a temperature
- If your child has a febrile convulsion, their body will go stiff, they will lose consciousness and their legs and arms may twitch.
- Put them in the recovery position immediately (see above) to keep their airway open.
- If it’s their first seizure or it lasts more than five minutes, take them to hospital or dial 999.
- Febrile convulsions are alarming to watch but are rarely dangerous and don’t have long-term effects.
Burns
- Put the burn under cold running water for at least 10 minutes to cool it down and reduce pain. It will seem like a long time, but 10 minutes is the minimum
- Burns can swell, so take off any tight clothes or jewellery
- Once it’s cool, cover the burn loosely with cling film or a plastic bag to prevent infection
- Take your child to A&E to be checked out.
Bleeding
- Clean the wound, under running water if possible, then pat it dry and put a plaster on top
- If it’s too big or deep for a plaster, use a sterile dressing or clean non-fluffy material with a bandage on top to hold the dressing in place. It needs to be firm enough to stop the bleeding (but not so tight that it stops circulation)
- If blood seeps through the bandage don’t take it off; put another dressing over the top
- If it soaks through the second, take them both off and start again with a new dressing, putting pressure on the wound
- If they are in shock (very pale, feeling faint), lie them down and raise their legs on cushions or pillows. Keep the wound raised above their heart, then take them to hospital
- If the wound has something embedded in it, such as glass, don’t remove it or apply pressure to it. Press either side of the wound to stem bleeding and take them to hospital